Chart Talk: Anesthesia Coding Conversations
Anesthesia Coding
-
We think we have everything mapped out.
We’ve set the goals.
We’re chasing the dream.
We’re finally stepping into the version of ourselves we’ve worked so hard to become.And then… life happens.
A health scare.
A family emergency.
An unexpected responsibility.
A season you didn’t plan for.Suddenly the dreams feel paused.
The momentum slows.
The plans get rearranged.It doesn’t seem fair.
It doesn’t feel fair.And if I’m being honest — I am feeling all of this right now.
I’m in a season of uncertainty.A season where things feel unclear.
Where plans feel fragile.
Where the future doesn’t feel as predictable as I’d like it to.Life isn’t always fair.
But what matters most is what happens next.
Do we stop?
Do we shrink back?
Do we tell ourselves, “Maybe this just isn’t my time”?Or do we adjust — without abandoning ourselves?
Here’s what I’m learning in this uncertain season:
You can pause without quitting.
You can shift without surrendering your vision.
You can take care of what needs tending without losing who you are becoming.Sometimes progress doesn’t look like forward motion.
Sometimes it looks like resilience.
Sometimes it looks like showing up quietly.
Sometimes it looks like surviving the week.We are often the only ones who can advocate for our dreams.
We are the only ones who can protect our purpose.But protecting your purpose doesn’t mean ignoring life. It means learning how to carry both.
The responsibility.
The interruptions.
The uncertainty.
And still — the dream.So how do you manage and not lose sight of it?
You redefine success in the season you’re in.
You give yourself grace.
You take the next small step instead of the giant leap.
You remind yourself that delay is not denial.And you refuse to let a hard season convince you that your calling no longer matters.
If you are in a season of uncertainty too, I want you to know — you are not alone.
You are not behind.
You are not failing.
You are navigating.And even in the uncertainty, growth is still happening.
Sometimes the strongest growth happens in the pauses.
And I’m choosing to believe that this season — even this one — still has purpose.
-
Cardiac Conditions and Anesthesia Coding Essentials
-
Tonight I had the privilege of presenting on anesthesia coding for the AAPC Chesapeake-Virginia Beach Chapter with approximately 390 attendees, and I am truly grateful.
Education and mentorship have always been passions of mine. Anesthesia coding is a specialty filled with nuance—where documentation details matter, clinical understanding is essential, and professional judgment plays a critical role. Being able to connect virtually through Microsoft Teams with a group of engaged coders who are eager to learn, ask questions, and sharpen their skills is something I never take for granted.
I remember when anesthesia coding felt overwhelming. The terminology, techniques, modifiers, blocks, time units—it can feel like learning a different language. That’s why I love sharing what I’ve learned over the years. If my experience can make the journey a little clearer or give someone more confidence in their coding decisions, then it is time well spent.
What stood out most during this presentation was the energy—even in a virtual setting. The thoughtful questions. The shared experiences. The willingness to discuss gray areas and documentation challenges openly. That’s what makes our coding community so strong—we learn from each other.
Networking with fellow professionals reminds me that we are not alone in this work. We all face payer audits, documentation gaps, evolving CPT® guidelines, and compliance challenges. But when we come together as a community, we grow stronger, more knowledgeable, and more confident.
To the AAPC Chesapeake–Virginia Beach Chapter—thank you for your hospitality, engagement, and commitment to excellence in coding. I am honored to have been part of your meeting.
And to every coder who continues to pursue education, mentorship, and growth—keep going. Your dedication matters more than you know.
Let’s keep the conversation going.
— Dianne
Chart Talk: Anesthesia Coding Conversations -
Growth doesn’t happen in the places where we feel safe, confident, and in control. If it did, we’d all be exactly where we want to be already. The truth—one we don’t always like to admit—is that real growth requires discomfort. It asks us to sit in uncertainty, to stretch beyond what feels familiar, and to risk feeling awkward, exposed, or even afraid.
And that’s hard.
Discomfort shows up in many forms. It’s the knot in your stomach when you speak up in a room where your voice hasn’t always been valued. It’s the hesitation before raising your hand for a new opportunity when you’re not sure you’re “ready.” It’s the quiet frustration of learning something new and realizing you don’t know as much as you thought you did. None of that feels good—but all of it matters.
We’re conditioned to avoid discomfort. We’re taught that if something feels hard, painful, or unsettling, it must be wrong. But what if discomfort isn’t a warning sign? What if it’s a signal that you’re standing at the edge of growth?
Every time you stretch beyond your comfort zone, you build resilience. You learn more about yourself—what you can handle, what you care about, and what you’re capable of becoming. Growth reshapes your confidence, not because things get easier, but because you get stronger.
Staying comfortable often means staying stuck. Familiar routines, familiar roles, familiar expectations—they can feel safe, but they can also quietly limit us. Discomfort, on the other hand, opens doors. It invites change. It challenges old beliefs and makes room for new possibilities.
That doesn’t mean you have to seek out chaos or overwhelm. Growth doesn’t require suffering—it requires courage. Courage to try. Courage to fail. Courage to be seen while you’re still figuring things out.
So if you’re feeling uncomfortable right now, pause before you push it away. Ask yourself what this moment might be teaching you. Ask whether this discomfort is stretching you toward the person you’re becoming.
Because comfort may feel good—but discomfort is where growth lives. And on the other side of it, you just might find the version of yourself you’ve been working toward all along.
— Dianne
Chart Talk: Anesthesia Coding Conversations -

*Anesthesia for hernia repairs in the lower abdomen not otherwise specified; younger than 1 year of age – 00834
Anesthesia for hernia repairs in the lower abdomen not otherwise specified; infants younger that 37 weeks gestation age at birth and younger than 50 weeks gestational age at time of surgery – 00836
-
Introduction
The sacroiliac (SI) joint is a well-recognized source of low back and buttock pain. Due to its complex anatomy and variable innervation, diagnosing SI joint–mediated pain can be challenging. Sacroiliac joint nerve blocks play a critical role in both diagnosing and treating this condition. CPT code 64451 was created to more accurately describe injections targeting the nerves innervating the sacroiliac joint rather than intra-articular injections.Anatomy and Innervation of the SI Joint
The sacroiliac joint receives sensory innervation primarily from the L5 dorsal ramus and the lateral branches of the S1, S2, and S3 sacral nerves. These nerves transmit pain signals from the posterior sacroiliac ligaments and joint capsule. Because innervation patterns can vary among patients, imaging guidance is essential to accurately target these nerves.Indications for SI Joint Nerve Blocks
Sacroiliac joint nerve blocks may be performed for both diagnostic and therapeutic purposes. Diagnostic blocks typically involve the injection of a local anesthetic to confirm the SI joint as the pain generator. A positive response is usually defined by significant temporary pain relief. Therapeutic blocks may include a corticosteroid to reduce inflammation and provide longer-lasting symptom relief.Procedure Overview
The procedure is typically performed with the patient in the prone position. After sterile preparation, fluoroscopic or CT imaging is used to guide needle placement to the L5 dorsal ramus and S1–S3 lateral branch nerves. Contrast is often used to confirm appropriate needle placement prior to injection of anesthetic and/or steroid medication. Imaging guidance is an inherent component of CPT 64451.Coding Considerations for CPT 64451
CPT 64451 describes injection(s) of anesthetic agent(s) and/or steroid into the nerves innervating the sacroiliac joint, including imaging guidance. This code should be reported only when all relevant nerves supplying the SI joint are targeted. If fewer nerves are injected, other codes such as 64450 may be more appropriate depending on documentation and payer policy.It is important to note that imaging guidance is included in the code descriptor and should not be reported separately. When the procedure is performed bilaterally, modifier -50 may be required unless payer-specific rules dictate otherwise. Documentation should clearly identify the nerves treated, laterality, imaging modality used, and medications injected.
Common Documentation Pitfalls
Incomplete documentation is a frequent cause of denied or downcoded claims. Common issues include failure to identify all nerves injected, lack of imaging confirmation, or vague descriptions such as “SI joint injection” without clarification of nerve versus intra-articular approach. Coders and auditors should carefully review procedure notes to ensure CPT 64451 is fully supported.Conclusion
CPT 64451 represents an important advancement in accurately coding sacroiliac joint nerve blocks. Understanding the anatomy, clinical intent, and documentation requirements is essential for compliant reporting. When properly supported, this code allows for accurate reimbursement while reflecting the complexity of the procedure performed.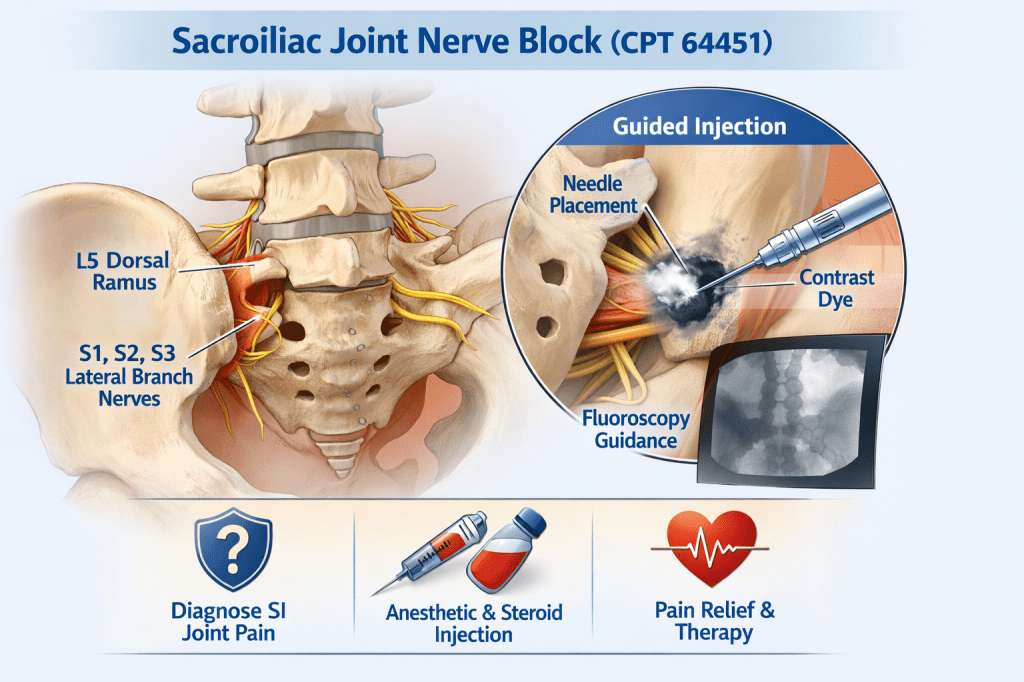
DISCLAIMER: Chart Talk: Anesthesia Coding Conversations is intended for educational and informational purposes only. The information presented reflects the sole interpretation and professional opinion of the presenter. It does not represent the views or official guidance of my employer, the Centers for Medicare & Medicaid Services (CMS), the American Medical Association (AMA), or any other regulatory or governing body.
Every reasonable effort has been made to ensure the accuracy of the information provided at the time of publication. However, coding guidelines, regulations, and payer policies are subject to change. It is the responsibility of the reader or participant to verify current guidance and apply professional judgment when making coding and billing decisions.
— Dianne
Chart Talk: Anesthesia Coding Conversations -
Today marks the first day of February, and with it comes American Heart Month—a crucial time to raise awareness about cardiovascular disease, the leading cause of death in the United States.
Since 1964, this national observance has focused on prevention through monitoring blood pressure, making heart-healthy nutrition choices, and staying physically active. Nearly 80% of cardiac events are preventable with healthy lifestyle changes and early intervention.
What This Means for Auditors & Coders
While clinicians focus on prevention and treatment, auditors and coders play a critical role behind the scenes. February is an ideal time for us to pause and take a closer look at the cardiovascular procedures we code and audit.
This is our opportunity to ensure coding is fully supported by documentation, aligned with current CPT, ASA, and ICD-10-CM guidelines, and compliant with payer and regulatory requirements.
Cardiac cases often involve complex procedures, multiple components, bundled services, and documentation that may imply details rather than clearly state them. That complexity can increase both compliance risk and missed revenue opportunities if we are not diligent.
A Coding Challenge for the Month
As part of American Heart Month, challenge yourself to review at least one cardiac procedure you frequently encounter. Revisit the documentation requirements, validate the coding guidelines, and ask yourself whether the record would withstand an external audit.
Let’s Start the Conversation
What type of heart-related procedure tends to trip you up the most when coding or auditing? Is it cardiac catheterizations, electrophysiology studies, CABGs, TEEs, or something else? Sharing these challenges helps us learn from one another and strengthen our coding accuracy.

DISCLAIMER: Chart Talk: Anesthesia Coding Conversations is intended for educational and informational purposes only. The information presented reflects the sole interpretation and professional opinion of the presenter. It does not represent the views or official guidance of my employer, the Centers for Medicare & Medicaid Services (CMS), the American Medical Association (AMA), or any other regulatory or governing body.
Every reasonable effort has been made to ensure the accuracy of the information provided at the time of publication. However, coding guidelines, regulations, and payer policies are subject to change. It is the responsibility of the reader or participant to verify current guidance and apply professional judgment when making coding and billing decisions.
— Dianne
Chart Talk: Anesthesia Coding Conversations -
Post-operative pain management continues to evolve, and ilioinguinal and iliohypogastric nerve blocks are commonly used regional techniques—particularly for lower abdominal procedures. While clinically effective, these blocks often raise coding and documentation questions, especially when they are performed together.
What Are Ilioinguinal and Iliohypogastric Nerve Blocks (CPT 64425)?
The ilioinguinal and iliohypogastric nerves originate from the L1 spinal nerve and provide sensory innervation to the lower abdominal wall, groin, and upper thigh region. Because of their close anatomical relationship, these nerves are frequently targeted together to manage post-operative pain.
Common procedures where these blocks may be used include:
• Inguinal hernia repairs
• Cesarean sections
• Appendectomies
• Gynecologic and lower abdominal surgeries
Single Injection vs. Two Separate Blocks
From a clinical standpoint, these nerves may be anesthetized with one injection at a single fascial plane or with two injections targeting each nerve individually. This distinction is critical for coding purposes.
Just because two nerves are involved does not automatically mean two separately billable blocks.
Coding Considerations
When ilioinguinal and iliohypogastric nerve blocks are performed, they are commonly reported as a single abdominal wall nerve block. When performed together via the same injection site, only one block is typically supported.
Separate reporting may only be considered when documentation clearly supports distinct injections, separate needle placements, and medical necessity for treating each nerve independently.
Documentation Elements to Look For
To support appropriate billing, the anesthesia record should include:
• Identification of the nerves blocked
• Laterality (if applicable)
• Technique used (ultrasound guidance or landmark-based)
• Number of injections and needle placements
• Purpose of the block (post-operative pain management)
Auditor’s Perspective
From an audit standpoint, the key is combining clinical reality with documentation support. If the record reflects one injection targeting both nerves with no distinction between separate techniques, reporting a single nerve block is generally appropriate.
This is another area where coding is not always black and white and where professional judgment plays an important role.
Final Thoughts
Ilioinguinal and iliohypogastric nerve blocks are effective tools in post-operative pain management, but they require careful review when it comes to coding and compliance. Understanding anatomy, technique, and documentation expectations helps ensure accurate reporting and audit defensibility.
Educational Use Disclaimer: This material is for educational purposes only and does not constitute billing or legal advice. CPT and coding guidance should always be applied in accordance with payer-specific policies and official guidelines.

DISCLAIMER: Chart Talk: Anesthesia Coding Conversations is intended for educational and informational purposes only. The information presented reflects the sole interpretation and professional opinion of the presenter. It does not represent the views or official guidance of my employer, the Centers for Medicare & Medicaid Services (CMS), the American Medical Association (AMA), or any other regulatory or governing body.
Every reasonable effort has been made to ensure the accuracy of the information provided at the time of publication. However, coding guidelines, regulations, and payer policies are subject to change. It is the responsibility of the reader or participant to verify current guidance and apply professional judgment when making coding and billing decisions.
— Dianne
Chart Talk: Anesthesia Coding Conversations -
In a perfect world, every medical record would contain clear, explicit language, neatly documented exactly the way coders want to see it. Every required element would be spelled out. Every box would be checked.
But those of us who live in the real world of coding know better.
Not everything in coding is black and white. Sometimes, it lives in the gray.
Professional coding is not about searching for magic words. It’s about understanding the medicine, the intent of the service, and the clinical story the record is telling. If coding were simply a word-search exercise, professional judgment wouldn’t matter — but it does.
There will be records where:
• The service is clearly performed, but the wording isn’t textbook
• The documentation supports the work, even if it doesn’t say it the way we wish it would
• The clinical picture makes sense when viewed as a whole, not as isolated phrases
Expecting every record to explicitly state every detail in the exact language we want before allowing a service to be coded or billed is unrealistic — and it doesn’t reflect how medicine is practiced.
That’s where professional judgment comes in.
Professional judgment means:
• Applying coding guidelines with clinical knowledge
• Reviewing the entire record — not just one sentence
• Understanding what is reasonably inferred versus what is truly missing
• Knowing when documentation supports a service and when it genuinely does not
This doesn’t mean we stretch the rules or ignore compliance. It means we apply them thoughtfully.
As auditors and coders, our role isn’t to deny everything that isn’t perfectly worded — nor is it to approve everything without scrutiny. Our responsibility is to balance compliance, accuracy, and clinical reality.
The gray area will always exist. The key is knowing how to navigate it responsibly.
Because at the end of the day, coding is not just about words on a page — it’s about understanding the story behind them.
Disclaimer:
Chart Talk: Anesthesia Coding Conversations is intended for educational and informational purposes only. The content shared does not constitute legal, billing, compliance, or reimbursement advice. Coding, billing, and reimbursement decisions should be based on official sources such as CPT®, ICD-10-CM, ASA guidelines, payer policies, and individual facility policies, as well as the specific documentation in the medical record. Users are encouraged to consult authoritative resources and/or their compliance department for guidance applicable to their organization.