Another week, another opportunity to learn something new in anesthesia pain management. This week’s spotlight focuses on an unusual but increasingly common technique used for post-operative pain control: fascial plane blocks—with a special focus on the Erector Spinae Plane (ESP) block.
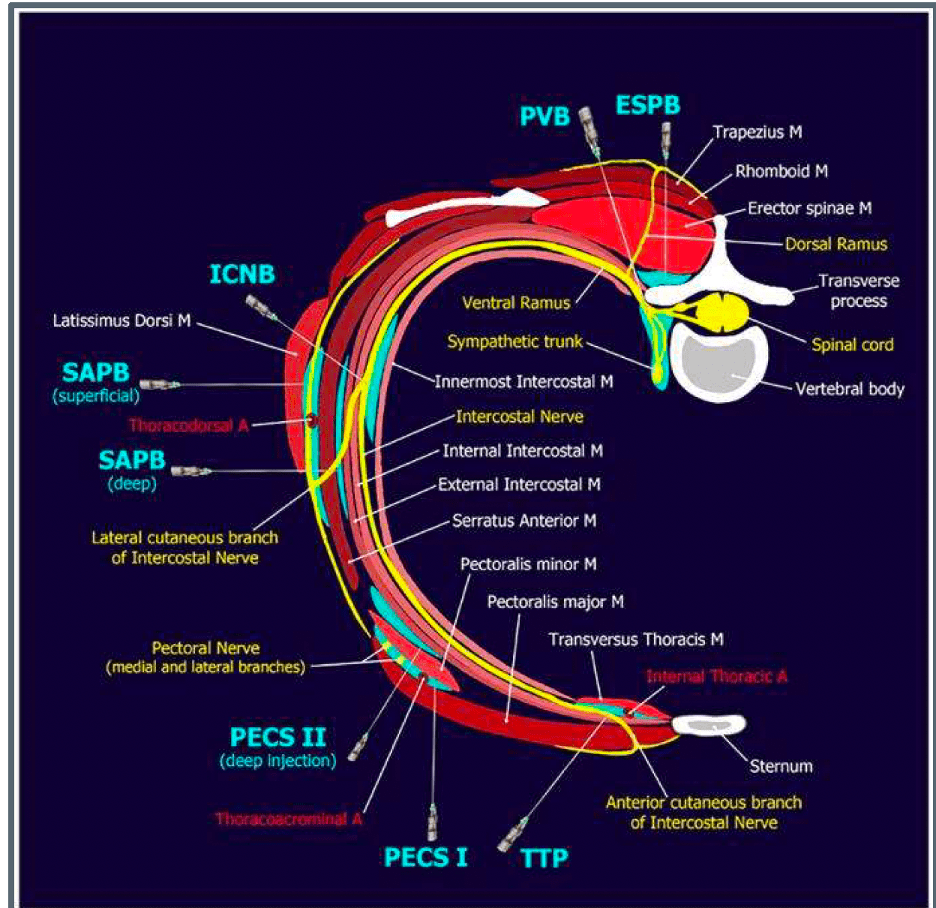
What Is a Fascial Plane Block?
Fascial plane blocks are regional anesthesia techniques where local anesthetic is injected between layers of fascia, rather than directly targeting a single named nerve. The medication spreads along the fascial plane, allowing coverage of multiple nerve branches and dermatomes.
Why the ESP Block Is Considered Unusual
The Erector Spinae Plane (ESP) block is considered unusual because it is performed at a location distant from the spinal cord and major nerve roots, yet it provides broad thoracic or lumbar analgesia. The block is placed deep to the erector spinae muscle, allowing cranio-caudal spread of anesthetic.
Common uses include:
- – Thoracic surgery
- – Rib fractures
- – Breast surgery
- – Abdominal and colorectal procedures
- – Spine surgery
Fascial Plane Block CPT Codes
Fascial plane blocks, including ESP blocks, are reported using the following CPT codes:
Thoracic (ESP) Fascial Plane Block Codes
CPT 64466 – Single injection, (unilateral)
CPT 64467 – Continuous catheter (unilateral)
CPT 64468 – Single injection, (bilateral)
CPT 64469 – Continuous catheter (bilateral)
Lumbar & Sacral (ESP) Fascial Plane Block Code
CPT 64999 – Unlisted Procedure
Documentation Requirements
To support billing for fascial plane blocks, documentation should clearly include:
- – Indication for post-operative pain control
- – Anatomical level(s): thoracic or lumbar
- – Single-shot versus continuous catheter technique
- – Laterality when applicable
- – Separate documentation from the surgical anesthesia record
- – Timing of the block (pre-op, intra-op for post-op pain, or post-op)
Common Audit Pitfalls
A frequent audit issue occurs when documentation simply states ‘ESP block performed’ without specifying the level, technique, or indication for post-operative pain. Incomplete documentation may result in denials or downcoding.
Closing Thoughts
Fascial plane blocks like the ESP block highlight how anesthesia pain management continues to evolve. For coders and auditors, understanding both the clinical intent and the CPT coding requirements is essential to ensure accurate reporting and compliance.
DISCLAIMER: Chart Talk: Anesthesia Coding Conversations is intended for educational and informational purposes only. The information presented reflects the sole interpretation and professional opinion of the presenter. It does not represent the views or official guidance of my employer, the Centers for Medicare & Medicaid Services (CMS), the American Medical Association (AMA), or any other regulatory or governing body.
Every reasonable effort has been made to ensure the accuracy of the information provided at the time of publication. However, coding guidelines, regulations, and payer policies are subject to change. It is the responsibility of the reader or participant to verify current guidance and apply professional judgment when making coding and billing decisions.
— Dianne
Chart Talk: Anesthesia Coding Conversations