Brachial Plexus – CPT 64415/64416
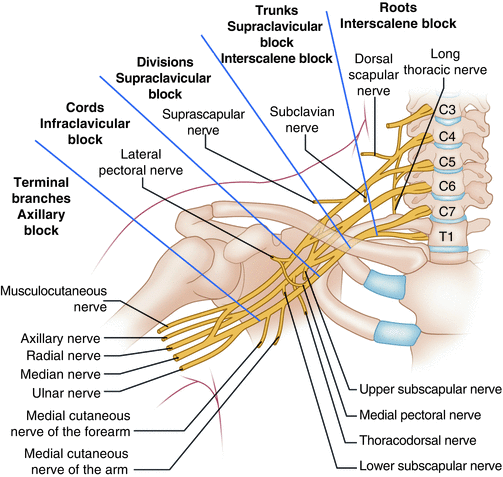
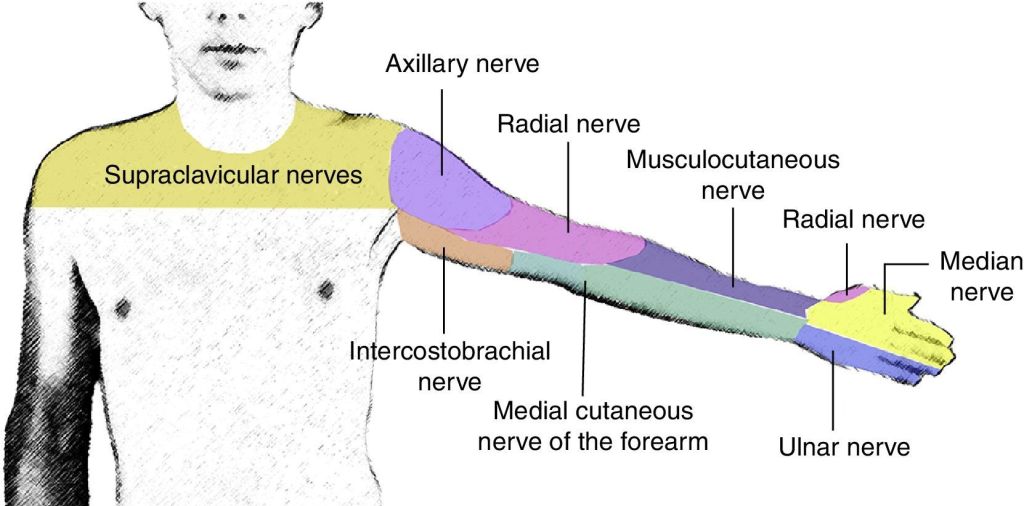
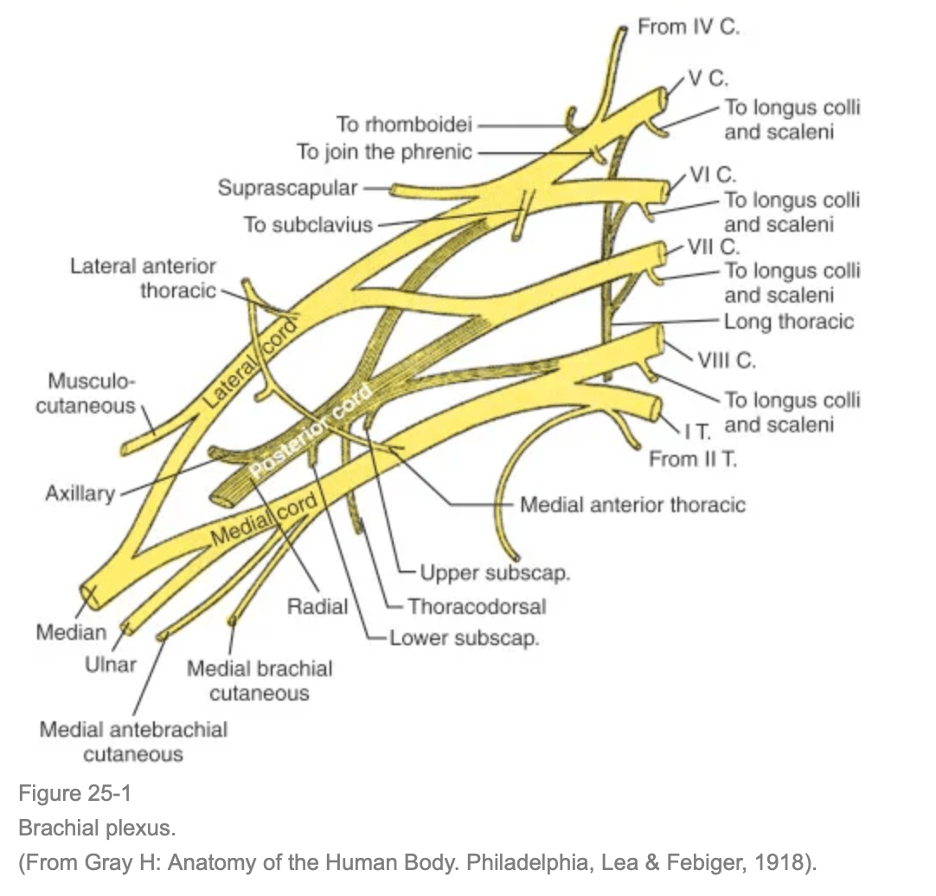
A brachial plexus nerve block is a regional anesthesia technique where local anesthetic is injected near the brachial plexus (a network of nerves for the arm) in the neck, above the collarbone, or armpit to numb the entire arm for surgery or to manage chronic pain, often as alternative to general. When brachial plexus is used for acute post op pain management
How does it work and its purpose?
- Blocks Pain: Temporarily stops pain and movement in the arm by numbing the nerve bundle.
- Surgical Anesthesia: Allows for awake or sedated surgery on the arm shoulder, or hand, avoiding general anesthesia side effects.
- Pain Management: Provides relief for arm and shoulder pain.
Common Approaches:
- Interscalene: Near the neck (between scalene muscles), best for shoulder surgery.
- Supraclavicular: Above the collarbone, excellent for elbow, wrist, and hand surgery.
- Infraclavicular: Below the collarbone
- Axillary: In the armpit, for hand, wrist, and forearm procedures.
Procedure & Guidance:
A doctor uses landmarks and often ultrasound to guide a needle to inject anesthetic near the nerves, sometimes placing a catheter for continuous pain relief. Ultrasound is bundled with code 64415/64416.
Axillary Nerve Block – CPT 64417
An ancillary nerve block is used for post op pain control, often for surgeries in the forearm, hand, wrist, or shoulder. It is billed for a single injection, providing pain relief by temporarily interrupting nerve signals, and requires specific documentation showing it’s separate from the main surgical anesthetic for. Post-op pain management.
How it Works for Post-Op Pain:
- The axillary nerve block targets the axillary nerve, a key nerve from the brachial plexus, located near the armpit.
- Anesthetic is injected near the nerve, often within a fascial compartment, to numb the area and block pain signals.
- It’s a common component of multimodal pain strategies to reduce reliance on opioids.
Common Usage Examples:
- Pain control after wrist fractures, elbow surgeries or shoulder surgeries.
- Part of a comprehensive approach (along with other blocks like the suprascapular nerve block) for shoulder analgesia.
* Axillary approach to Brachial Plexus is coded as 64415 (typically shoulder cases). True Axillary Blocks target the Axillary nerve and are coded 64417 (typically forearm/wrist/hand procedures). Review the block note to confirm the targeted nerve
Suprascapular Nerve Block – CPT 64418
A suprascapular nerve block (SSNB) is a highly effective technique for managing acute postoperative shoulder pain, especially after arthroscopic procedures, by injecting local anesthetic around the nerve that supplies about 70% of the shoulder’s sensation, significantly reducing opioid needs, nausea, and pain scores, and allowing for earlier rehabilitation. It’s a safe alternative for patients with lung issues who can’t have general nerve blocks and can be combined with other blocks (like axillary) for even better results, though it’s less effective than a full interscalene block but offers better safety.
How It Works:
- Injection: A doctor injects a local anesthetic (like lidocaine/bupivacaine) near the suprascapular nerve, often guided by ultrasound for precision.
- Pain Interruption: The anesthetic temporarily blocks pain signals from the shoulder joint to the brain.
- Safer Alternative: Avoids phrenic nerve block (diaphragm paralysis) seen with interscalene blocks, making it ideal for patients with lung disease, notes ASRA Pain Medicine.
When It’s Used:
- Arthroscopic shoulder surgeries (rotator cuff repair, etc.).
- Chronic shoulder pain (arthritis, frozen shoulder, tendonitis).
Techniques:
- Posterior Approach: Common, targeting the nerve at the suprascapular notch.
- Anterior Approach: Also described and effective.
- Combination: Often paired with an axillary nerve block (SSNB+ANB) for comprehensive pain relief, though it may not surpass a standard interscalene block (ISB) but offers fewer side effects like breathing issues.
Suprascapular Nerve Block – CPT 64418
A suprascapular nerve block (SSNB) is a highly effective technique for managing acute postoperative shoulder pain, especially after arthroscopic procedures, by injecting local anesthetic around the nerve that supplies about 70% of the shoulder’s sensation, significantly reducing opioid needs, nausea, and pain scores, and allowing for earlier rehabilitation. It’s a safe alternative for patients with lung issues who can’t have general nerve blocks and can be combined with other blocks (like axillary) for even better results, though it’s less effective than a full interscalene block but offers better safety.
How It Works:
- Injection: A doctor injects a local anesthetic (like lidocaine/bupivacaine) near the suprascapular nerve, often guided by ultrasound for precision.
- Pain Interruption: The anesthetic temporarily blocks pain signals from the shoulder joint to the brain.
- Safer Alternative: Avoids phrenic nerve block (diaphragm paralysis) seen with interscalene blocks, making it ideal for patients with lung disease, notes ASRA Pain Medicine.
When It’s Used:
- Arthroscopic shoulder surgeries (rotator cuff repair, etc.).
- Chronic shoulder pain (arthritis, frozen shoulder, tendonitis).
Techniques:
- Posterior Approach: Common, targeting the nerve at the suprascapular notch.
- Anterior Approach: Also described and effective.
- Combination: Often paired with an axillary nerve block (SSNB+ANB) for comprehensive pain relief, though it may not surpass a standard interscalene block (ISB) but offers fewer side effects like breathing issues.
DISCLAIMER: Chart Talk: Anesthesia Coding Conversations is intended for educational and informational purposes only. The information presented reflects the sole interpretation and professional opinion of the presenter. It does not represent the views or official guidance of my employer, the Centers for Medicare & Medicaid Services (CMS), the American Medical Association (AMA), or any other regulatory or governing body.
Every reasonable effort has been made to ensure the accuracy of the information provided at the time of publication. However, coding guidelines, regulations, and payer policies are subject to change. It is the responsibility of the reader or participant to verify current guidance and apply professional judgment when making coding and billing decisions.
— Dianne
Chart Talk: Anesthesia Coding Conversations
Leave a comment