The start of a new year is the perfect time to reset habits, refine processes, and strengthen the foundation of accurate anesthesia coding. When it comes to clean claims and compliant billing, one truth remains constant:
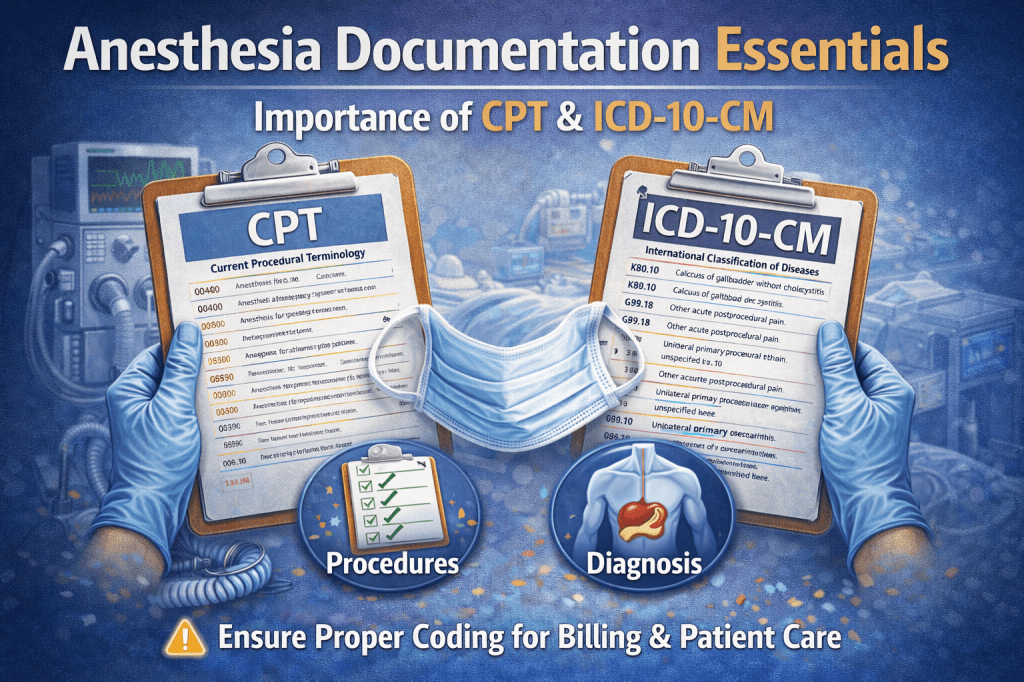
CPT accuracy starts with ICD-10-CM.
While anesthesia coding often focuses heavily on time, units, and modifiers, none of that matters if the underlying diagnosis does not clearly support the service provided.
🔗 Why ICD-10-CM Is the Foundation of Anesthesia CPT Coding
Every anesthesia claim tells a story—and ICD-10-CM codes set the stage. They explain why anesthesia was medically necessary and how complex the patient’s condition truly was.
Strong diagnosis documentation supports:
- Appropriate anesthesia CPT code selection
- Medical necessity for the procedure
- Risk stratification and ASA status
- Audit defensibility
Without clear, specific diagnoses, even perfectly calculated anesthesia time can be challenged.
📌 Common Documentation Gaps That Impact CPT Accuracy
Many anesthesia documentation issues are not coding errors—they’re documentation gaps. Some of the most common include:
- Vague diagnoses such as “abdominal pain” or “back pain” without specificity
- Chronic conditions listed in the history but missing from the final assessment
- Comorbidities documented but not linked to anesthesia risk
- Discrepancies between the surgeon’s diagnosis and the anesthesia record
These gaps make it difficult to assign accurate ICD-10-CM codes, which can ultimately affect CPT code support and reimbursement.
🧠 Linking Diagnosis → Procedure → Anesthesia CPT
Accurate anesthesia coding requires alignment across the entire record:
- Diagnosis (ICD-10-CM)
What condition or disease prompted the procedure? - Procedure (Surgical CPT)
What service was performed that required anesthesia? - Anesthesia CPT Code
Does the anesthesia code align with the procedure and patient condition?
When these elements tell the same story, claims are stronger and audits are easier to defend.
⚠️ Diagnosis Specificity Matters More Than You Think
ICD-10-CM specificity isn’t just a surgical concern—it directly impacts anesthesia services. Detailed diagnoses help reflect:
- Increased patient risk
- Complexity of care
- Need for heightened monitoring or intervention
For example, documenting controlled vs. uncontrolled conditions, acute vs. chronic status, or complications can make a meaningful difference in how the case is reviewed.
📋 Documentation Tips for a Strong Start to 2026
As we move into the new year, consider these best practices:
- Ensure diagnoses are carried through from pre-op to final assessment
- Capture all clinically relevant comorbidities impacting anesthesia care
- Encourage consistency between surgeon and anesthesia documentation
- Audit records for diagnosis clarity—not just time and units
Small improvements in documentation can have a big impact on CPT accuracy.
💬 Let’s Start the Conversation
As we begin 2026, take a moment to reflect:
👉 If you could improve one anesthesia documentation issue this year, what would it be?
Drop a comment, reply to this post, or share your experience. Your insight may help another coder, auditor, or provider strengthen their documentation practices.
Here’s to a year of clean claims, strong documentation, and continued growth in anesthesia coding.
DISCLAIMER: Chart Talk: Anesthesia Coding Conversations is intended for educational and informational purposes only. The information presented reflects the sole interpretation and professional opinion of the presenter. It does not represent the views or official guidance of my employer, the Centers for Medicare & Medicaid Services (CMS), the American Medical Association (AMA), or any other regulatory or governing body.
Every reasonable effort has been made to ensure the accuracy of the information provided at the time of publication. However, coding guidelines, regulations, and payer policies are subject to change. It is the responsibility of the reader or participant to verify current guidance and apply professional judgment when making coding and billing decisions.
— Dianne
Chart Talk: Anesthesia Coding Conversations
Leave a comment